When it comes to hip surgery for the elderly, faster may be better
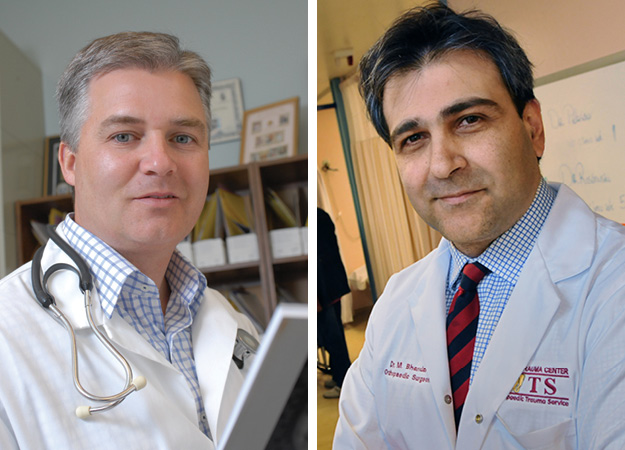
According to a new study led by Dr. P.J. Devereaux (left) and Dr. Mohit Bhandari, time is of the essence for elderly patients awaiting hip surgery. Having a procedure performed within six hours of an injury can significantly reduce major health complications.
The speed of surgery after a hip fracture may have a significant impact on outcomes for older patients, and faster may be better, say researchers at McMaster.
The study was published Monday in the Canadian Medical Association Journal (CMAJ).
For seniors, hip fractures can cause serious complications that may result in death or admission to long-term care facilities. Hip fractures cause pain, bleeding and immobility, and activate patients’ coagulation and stress systems which can lead to medical complications in people awaiting surgery.
In Canada and many other countries, wait times for hip surgery can be 24 hours or longer, mainly because of pre-surgery clearance procedures and lack of operating rooms.
During the McMaster-led study — which involved 60 people aged 45 or older in Canada and India — half received accelerated hip surgery within six hours, and half received the standard care of surgery 24 hours after diagnosis.
Among patients receiving standard care, 47 per cent suffered a major complication of death, heart attack, stroke, pneumonia, blood clot or major bleeding. However, only 30 per cent of the patients in the accelerated surgery group suffered one of these complications.
“We believe that the shortest time possible to treatment may provide the greatest potential for benefit, as is the case in acute heart attack and stroke,” said Dr. P.J. Devereaux, an associate professor of medicine and epidemiology at the Michael G. DeGroote School of Medicine, and co-principal investigator of the pilot trial.
“This pilot provides encouraging evidence that accelerated surgery may substantially improve outcomes in these patients,” added Dr. Mohit Bhandari, a surgery professor at McMaster and co-principal investigator.
The research was funded by an operating grant from the Academic Health Science Centres (AHSC) Alternative Funding Plan (AFP) Innovation Fund Grant of Ontario and an investigator grant from Octapharma Canada Incorporated. A full-scale trial is planned for 2014, and interested academic researchers are invited to join the trial.

