Study finds HIV not as infectious soon after transmission as previously thought
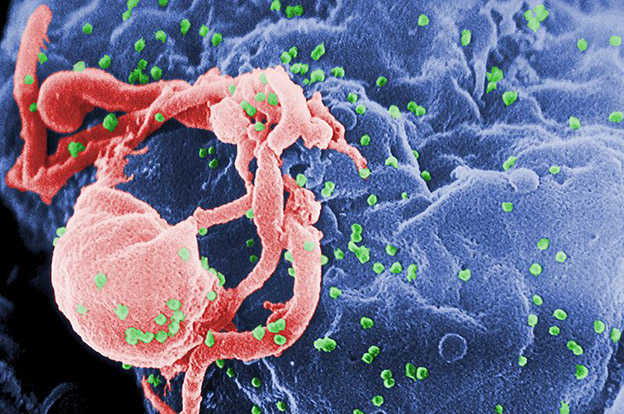
Scanning electron micrograph of HIV-1 budding (in green) from cultured lymphocyte. A new study has found that people who recently contracted HIV may not be as highly infectious as previously thought.
People who only recently contracted HIV may not be as highly infectious as previously believed, a new analysis conducted by researchers at McMaster, the University of Texas at Austin and Yale University has found.
The finding has implications for public health approaches to controlling the spread of HIV, including decisions about giving more patients antiretroviral drugs before the onset of AIDS.
The study was published today in PLoS Medicine. Jonathan Dushoff, an associate professor of biology and an investigator with the Michael G. DeGroote Institute for Infectious Disease Research at McMaster, is one of the authors, with principal author Steve Bellan and co-authors Lauren Ancel Meyers of the University of Texas at Austin, and Alison Galvani of Yale University.
“The current study provides the best available estimates of the relative infectiousness of early-stage patients,” said Dushoff.
He added that researchers already know that state-of-the-art drug treatment for HIV is very good both for protecting patients and for reducing transmission risk; in effect protecting their partners as well.
“An open question is how much potential there is for treatment programs to protect whole populations from HIV, by interrupting transmission of the virus,” said Dushoff. “An important concern here is how infectious early-stage HIV patients are because it will be extremely difficult to find and treat most patients while they are still in the early stage.”
Within a few weeks of transmission, people who are HIV-positive enter an acute phase of infection, a period of several months when levels of the virus in the bloodstream spike. The acute phase is followed by a roughly 10-year chronic phase of infection that precedes AIDS.
The acute phase has been associated with elevated risk for passing the virus to others, with previous research suggesting that the risk is far greater than even expected based on the viral spike. Researchers have argued that a large portion – or even the majority – of HIV transmission may arise from individuals who have just been infected themselves.
But the new study finds that previous estimates of infectivity during this acute phase are likely to be too high. In fact, today’s report suggests one of the most commonly cited estimates could be as much as 20 times too high.

“We found that passing HIV to another person isn’t as likely to happen during this stage as people have been assuming for many years,” said Bellan. “That fact would be cause for optimism when it comes to novel interventions that aim to curb HIV’s spread. It could also have implications for the way that communities direct public health resources, leading to more effective approaches that save more lives.”
Estimating infectivity during acute-phase HIV is widely known to be difficult, and only one study, involving heterosexual couples in Rakai, Uganda, has ever directly measured the infectiousness during this stage of HIV.
The new analysis used two approaches to estimate additional risk of transmission during the acute phase.
One approach drew upon data in the Rakai study, but accounted for certain differences among the couples that were not factored into earlier analyses.
The other approach looked at the trajectory of virus levels during the acute phase and the known relationships between viral load and infectivity.
Both approaches found a higher risk of transmission during the acute phase of HIV, but the amount of added risk to public health came out to the equivalent of five extra months of chronic-phase infectivity. By contrast, the most commonly cited earlier estimates calculated excess risk during the acute phase as equivalent to a period in the range of 31-141 extra months of chronic-phase infection.
Each year an estimated two million people worldwide become newly infected with HIV, the disease that causes AIDS. According to the study, treating HIV-infected individuals with antiretroviral drugs not only prevents AIDS, but also makes them unlikely to infect others.
In the past five years, policy has consequently shifted towards programs that aim to keep HIV infections from spreading across a population by administering antiretroviral treatment as a preventive strategy. However, individuals can only be treated once they are tested and diagnosed, and individuals rarely get tested within the first few months after infection.
Because of this lag between infection and diagnosis, these “treatment as prevention” programs are unlikely to prevent transmission from acutely infected individuals, and many have thought that this strategy will fail to prevent much of HIV’s spread.
The new analysis suggests a better outlook than previously thought, however, given that it is less likely that newly infected patients could undermine the strategy’s impact. By contrast, programs focused entirely on early identification of the disease may not be as cost-effective as once thought for controlling HIV’s spread.
This research was funded by the National Institute of Health and the J.S. McDonnell Foundation.
